
China Baby Milk Scandal – 2008
A parent’s worst nightmare came true for thousands of families in China in 2008 when

A parent’s worst nightmare came true for thousands of families in China in 2008 when

The multinational company Trafigura did a nifty deal in 2006, buying a large amount of

In March 2006 six healthy men, all under the age of 40, signed up as
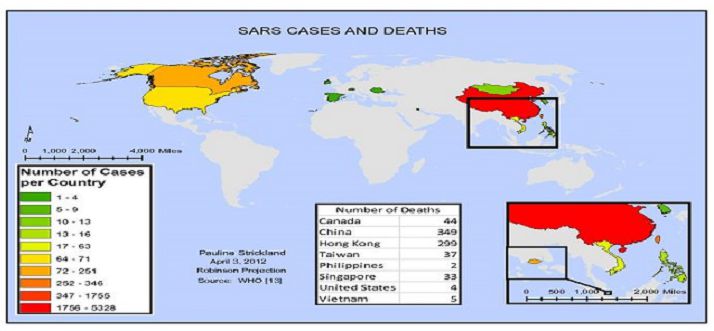
Towards the end of 2002 reports began to emerge from China of a virulent and

Meningococcal meningitis is a bacterial infection of the slender lining that envelops the spinal cord

When the Zaragoza Clinic’s electron accelerator malfunctioned and was repaired in early December 1990, it

In scientific terms Bovine Spongiform Encephalopathy (BSE) and variant Creutzfeldt-Jakob Disease (vCJD) are Transmissible Spongiform

Nothing goes to waste where people are living on the breadline, and few opportunities to

It is difficult to pinpoint exactly when the AIDS epidemic began. The first death assumed

It started with the death of eight-year-old Jaime Garcia in his mother’s arms on the

Described as ‘the worst treatment disaster in the history of the NHS’, the tainted ‘Hemofil’
After a series of disastrous harvests in the late 1960s, Saddam Hussein applied for an
Images of the effects of Thalidomide are firmly etched into the public consciousness. What was

Poliomyelitis is a peculiarly nasty, highly contagious disease of the central nervous system that all

Doctors first noticed something strange in the Japanese coastal town of Minimata towards the end
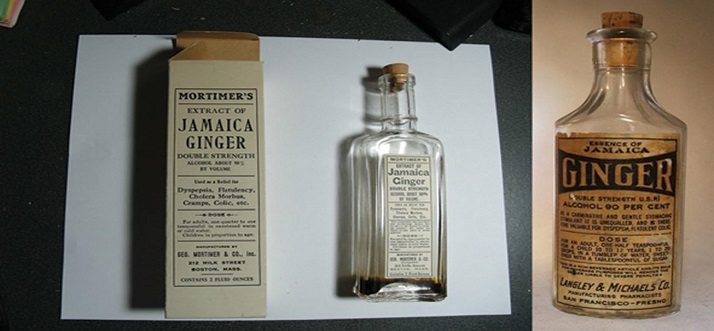
It goes by the name of ‘potcheen’ in Ireland, ‘hooch’ or ‘moonshine’ in North America
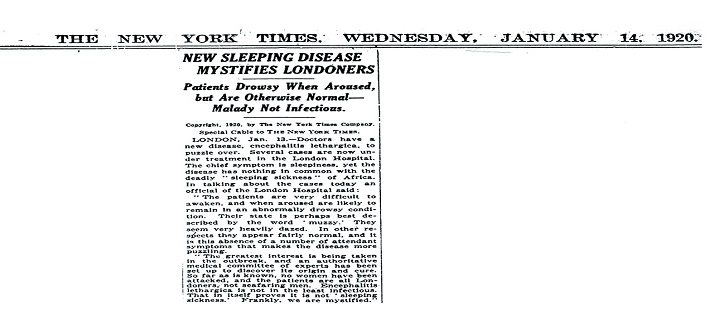
The ‘sleeping’ or ‘sleepy’ sickness that swept the world in the 1920s had nothing in

Despite its name, the flu pandemic of 1918 did not start in Spain. In fact
Do you think it’s ok to shoot the leaders of America? We all know what
How clean is the air you breathe? According to a new report, a mere seven
Can the crime rate be reduced in any of these cities? Living in cities with
Chicago is a destination known for its summer fun, sports, entertainment, food scene, diversity, and